
As we celebrate a new addition to the Stepped Care 2.0® (SC2.0) book series, we are also reflecting on the journey of system transformation so far. In this first article from our Founding Thinkers Space, Dr. Gillian Berry shares the early successes of SC2.0, and how the model invites and supports change agents to tackle challenges head-on.
By Dr. Gillian Berry
Over the past few months, we’ve been hearing a familiar question from partners and new contacts alike: “What exactly is Stepped Care 2.0, and how does it work in practice?” As we expand Stepped Care 2.0® (SC2.0) to jurisdictions across North America and internationally, we wanted to take a moment to reflect on where the model started, what we’ve learned along the way, and what makes it transformational.
At Stepped Care Solutions, our journey toward mental health system transformation began with a conundrum, but at the time, we did not realize how vital conundrums would become to the implementation of SC2.0.
In the early 2000s, Peter Cornish, our founder, then a newly minted administrator at a university counselling service, observed a contradiction. Students often waited three or four weeks for appointments, while urgent walk-in spots were frequently left unused. Like many services, including emergency departments, it made sense to schedule staff for potential crises. But unlike emergency departments, urgent mental health cases were infrequent.
The Student Wellness and Counselling Centre was spending a significant amount on on-call availability, yet students ready to proactively address their mental health were facing long wait times. No one, including Peter, thought it was a good idea to shut down the urgent on-call system, but at the same time, there were real challenges to providing accessible basic care. The current system was expensive and left many students without timely, proactive support. And, there was no money to hire additional staff. A conundrum indeed.
This challenge led to a pivotal realization: what if, instead of choosing between urgent and basic care, the system was redesigned to do both? Rather than either-or thinking, adopting a both-and mindset allowed us as practitioners to reimagine care structures where urgent and non-urgent supports could co-exist in a single flexible framework. That early idea eventually grew into what we now know as Stepped Care 2.0.
A Paradigm Shift Rooted in Access and Flexibility
In the book Stepped Care 2.0: A Paradigm Shift in Mental Health, Peter introduced a key idea: that mental health systems must evolve beyond rigid, hierarchical structures into an adaptive, client-centred continuum. The driving question became: How might well-being be reimagined everywhere? As with all big hopeful ideas, this one appears characteristically unrealistic, somewhat naive, yet universally enticing. It was an impossible possibility.
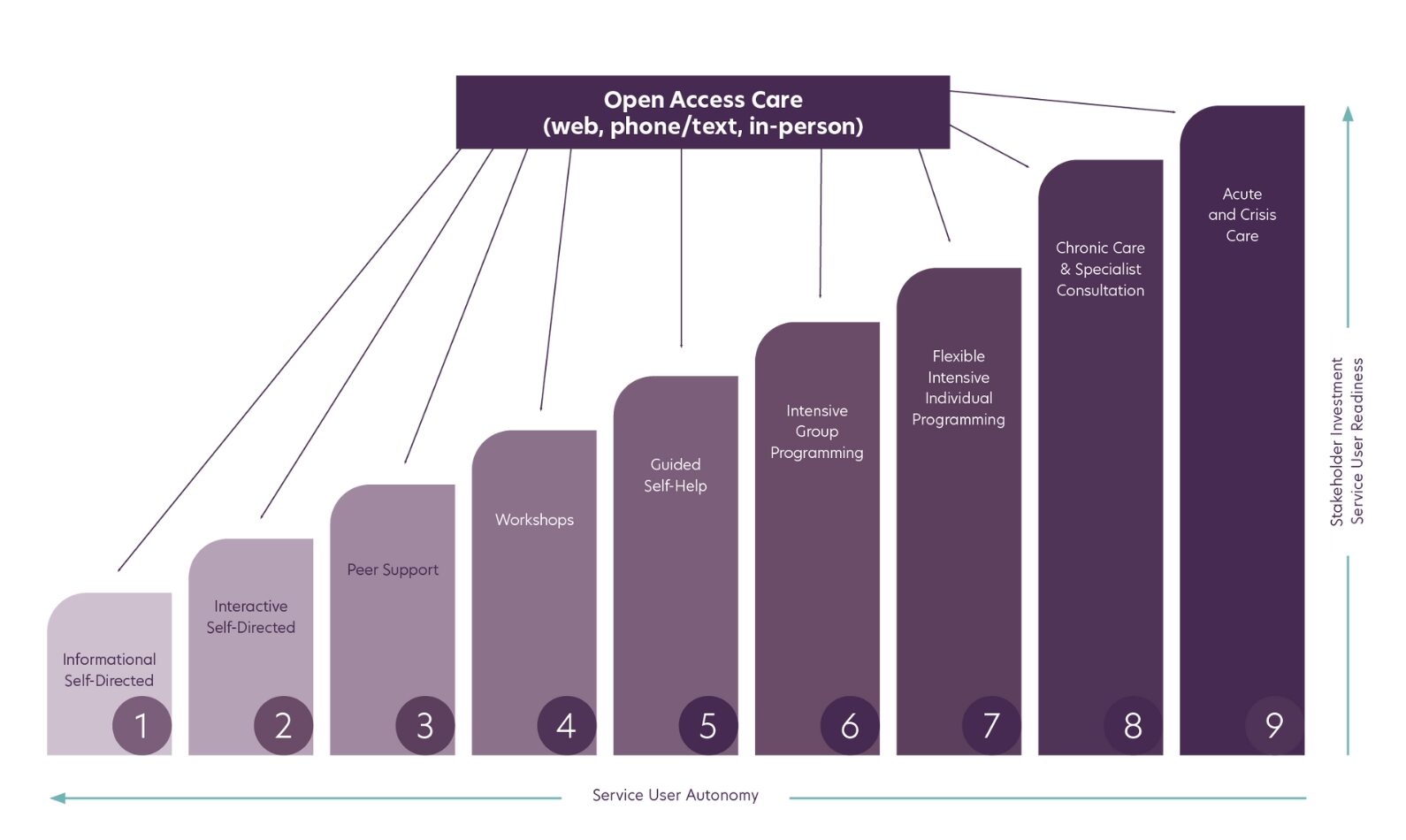
The traditional model—built around high-intensity, specialized services—has its place. But for many, it isn’t the best fit. The assumption that everyone needs long-term therapy or psychiatric care overlooks the value of brief, lower-intensity supports. Many people benefit from digital tools, peer support, or brief clinical interventions at just the right time.
Stepped Care 2.0 emerged as a response to this gap. Rather than asking people to wait for weeks—or even months—for a one-size-fits-all solution, SC2.0 meets people where they are, matching the level of support to their needs in the moment.
The counselling staff could be available for drop-ins for both urgent and non-urgent care at the same time. Although Peter did not know it at the time, this was the beginning of a more holistic system-level redesign process, bringing seemingly opposed care components together to create something greater than the sum of the parts. It began by integrating urgent care with basic care. It progressed to include self-help, peer support, health promotion, and population health interventions together in an integrated system.
The Birth of a New Mental Health Paradigm
Mental health care has historically been designed around high-intensity interventions provided by specialized professionals. And why not? We all deserve the best. But upon closer inspection, might we ask, “Is it the best in all circumstances?” Of course, intensive or long-term treatment can be effective, but what about other methods of support? And how realistic is it that there would ever be enough specialists to serve all in need of care?
The assumption has long been that most individuals struggling with their mental health require a course of psychotherapy (usually 8-16 sessions at a minimum) or psychiatric medication to find relief. However, this well-established model has led to widespread inefficiencies, inaccessibility, and frustration. The reality we are discovering is that many individuals need more timely, lower-intensity support rather than either long-term or intensive clinical treatment.
SC2.0 arose from the recognition that established mental health models were failing vast segments of the population. The one-size-fits-all approach—where individuals wait weeks, or even months, for 50-minute therapy sessions—simply wasn’t sustainable. Instead, Peter and our small group of mental health innovators envisioned a system that flexibly matched individuals to the level of care they needed at the moment they sought help, whether that be digital resources, peer support, brief interventions, or specialized therapy.
Learning from Early Adoption and Momentum
Early implementation of SC2.0 saw immediate gains: reduced wait times, increased access, and improved client and provider satisfaction. The framework resonated with early adopters—those ready to embrace innovation and data-driven decision-making in mental health care.
But not all implementation efforts were smooth. Many licensed providers, accustomed to familiar workflows and professional roles, raised valid questions about the shift. Some policymakers were also hesitant to commit to full implementation. Those professionals asked, “Do we really need all the elements of the framework?” Others expressed concern that, by not offering the established “gold standard” of traditional therapy to every client, the new model was about cutting costs, not expanding care options.
Our initial instinct, as pioneers and the creators of SC2.0, was to defend the framework—to argue that we were broadening access, not replacing anyone’s work. But we soon recognized that defensiveness would not help us grow. We needed to listen better.
Writing Stepped Care 2.0: A Paradigm Shift in Mental Health was a milestone for Peter (he admits he never thought he was capable of it), “…a bold, big plan for personalized population health,” John Norcross wrote in the Foreword. But Peter felt differently. He knew the book wasn’t a complete guide with all the necessary ingredients for transforming a system. While it could well be a good place to start the work, he had a nagging feeling that something important was missing.
While undeniably exciting—with meaningful transformations unfolding across various jurisdictions—SC2.0 creators embraced an intentional practice to pause, observe, and engage with the emerging ripples of dissent. Listening with what one psychologist called a ‘third ear’ (Reik, 1948), this required hearing the hard and uncomfortable things without getting defensive. In the midst of change, we found that challenges were less obstacles and more opportunities waiting to be explored with curiosity and enthusiasm. These proverbs rang true:
- Where there’s a problem, there’s a puzzle to solve.
- Adversity is the playground of innovation.
- Difficulties are the stepping stones to progress.
The full extent of the challenges became clear to us. We deliberately acknowledged the resistance, paid attention to what was missing in our framework, and listened deeply with the goal of refining the model with input from those in opposition.
True and sustainable transformation is hard. It requires a mix of bold leadership, thoughtful change management strategies, and a combination of empathy, listening, and radical candour. As John Norcross warns in the Foreword to Stepped Care 2.0: A Paradigm Shift in Mental Health, “If you intend minor tweaking of your mental health services, then this is decidedly not the book for you.”
SC2.0 invites change agents to practice diplomatic disruption. This means listening carefully and tackling challenges head-on, not ignoring or pretending they don’t exist. For transformation to work, it is essential to show up with humility and acknowledge struggle while cultivating hope and a spirit of discovery.
Find “Synergy: The Healing Energy Guiding Stepped Care 2.0”, and all books in the SC2.0 series, at Springer Publishing, as well as Amazon and Indigo.
For more information on SC2.0 and how it can transform mental health and wellness systems and service delivery, contact our implementation experts to explore your opportunities.

