Stepped Care 2.0: A framework for more accessible, effective mental health and substance use health care systems
Why Stepped Care 2.0?
Mental health care providers face ongoing challenges in improving service accessibility and efficiency. High demand, long waitlists, resource-intensive assessments, geographical and cultural barriers, and outdated systems hinder progress. Despite these obstacles, many leaders, practitioners, and educators remain committed to enhancing care delivery for all and fostering a more inclusive and effective mental health and substance use health landscape.
SC2.0 is an innovative and transformative model of organizing and administering resources that fundamentally reimagines mental health and substance use health care systems from the inside out. At its core, the SC2.0 model positions people seeking access to services and resources as active participants in their care journey. Our focus is on assessing, developing and enhancing service delivery and technology systems that enable people to access the type of support that works best for them, when they need it.


No one size fits all
Our approach to system reimagination is grounded in the 10 principles that drive us toward our vision of Wellbeing Everywhere. We collaborate with organizations, communities and their stakeholders to enable and enact better access and outcomes.
We shift away from the status quo medical model framework in two significant ways:
1
We work with partners to develop and deliver person-centric, culturally sensitive systems of care that include the communities they serve.
2
Identifying and developing system responses that prioritize open and immediate access, choice, prevention, mental health and substance use literacy, and empowerment.
Our work is globally recognized for leadership, innovation and technical dexterity in implementation science, evaluation and monitoring, knowledge exchange, coalition building, ecosystem development, and clinical expertise.
The outcome of our approach is remarkable

Immediate and aligned access to services
Organizations can measure, adjust and communicate the impact of their work
Changes are based on data and evidence informed considerations

Empower people accessing services, employees and stakeholders
Build and enhance an interconnected approach to mental health care
An effective and meaningful stepped approach with proven care seeker satisfaction
Intro to SC2.0
Quick and easy access to many regional resources and services
- Reduced wait lists in three provinces by 62% (Harris-Lane et al, 2022; MHCC, 2019)
- Reduced average wait time for individual counselling, e.g., from 15 days to 3 days (Cornish et al. 2017)
Systems incorporate formal and informal supports, that are culturally safe and relevant
- Increased rates of agreement that the service was helpful (Goodman, 2021)
- Increase in the percentage of students who agree that counselling was sensitive to their ethnicity, sexual orientation and other cultural differences (Goodman, 2021)
An expanded and diverse workforce with a community- wide approach
- Increased appointment attendance (Cornish et al. 2017)
- Increased rates of agreement that the service was helpful (Goodman, 2021)
A care-first approach that puts people’s needs first and recognizes their strengths and capacities
- Close to 80% of clients reported that low-intensity options (e.g., e-mental health tools) met at least some of their needs (MHCC, 2019)
- 92% of clients were satisfied with a One-at-a-time (OAAT) counselling session to address their problems (Harris-Lane et al, 2022)
Digital expertise
We have developed extensive expertise in the co-development, delivery, and maintenance of digitally-enabled mental health system innovations at all scales – national, regional, and within institutional/organizational settings.
Our ability to tailor approaches and plans to specific contexts is a unique strength. The large and complex initiatives we lead and support, are made possible through our focus on partnership, innovation, training and community engagement.
How do we do this?
The implementation of SC2.0 begins with a careful assessment of the present system. Understanding strengths and challenges with existing resources, services and programming informs the next steps of considering services to be offered and strengthened, such as e-mental health interventions, self-guided support, peer support, group programming and in-person therapy. Service options align with the structure and number of steps appropriate to the setting. Looking at the community and larger supports and services is a critical part of informing shifts and changes.

Stepped Care Solutions approach
As a mission-driven, not-for-profit organization committed to system change, we prioritize lean resource allocation to maximize value and impact across systems large or small. This approach benefits our partners, communities, and taxpayers alike, resulting in a strong ROI, increased capacity, and a lean, results-driven environment that exemplifies care.
In a nutshell, the SC2.0 framework facilitates a system that offers increased access to care at various levels of intensity. Uniquely, care seekers have informed choice of an extended range of services based on individual needs, preferences and readiness to engage.
Unlike other approaches, programming is adjusted, in part, based on the response and preference of those seeking services, rather than relying on symptom-based, one-size-fits-all treatment protocols. Both care seekers and service providers engage in continuous feedback on progress, empowering each to collaborate on care options and decision-making. By keeping continuous improvement top of mind, we can proactively respond to glitches, challenges and successes.
OPEN ACCESS
SC2.0 promotes flexible options and access, to help care seekers at their point of need and stage of readiness, with minimal assessment. People experience support immediately.
SYSTEMATIC REACH
A SC2.0 designed system considers the population it is to serve and integrates a full continuum of services, from prevention/promotion to acute care.
CONTINUOUS IMPROVEMENT
The foundation of the SC2.0 approach is based on continuous improvement to benefit systems, providers and people seeking care.
CO-DESIGNED
SC2.0 facilitates a system of care that is co-designed with the voices of care seekers, providers, organizations and the community. Our co-design process is rooted in principles of synergy. Every step of the way, care options are co-designed to redress inequities within current systems of care.
CLIENT-CENTRIC
SC2.0 is recovery-oriented and client-centric, embracing synergy; our approach to diversity and inclusion. Applying these principles helps ensure that the needs and experiences of different groups of people are reflected, resulting in more inclusive and responsive approaches.
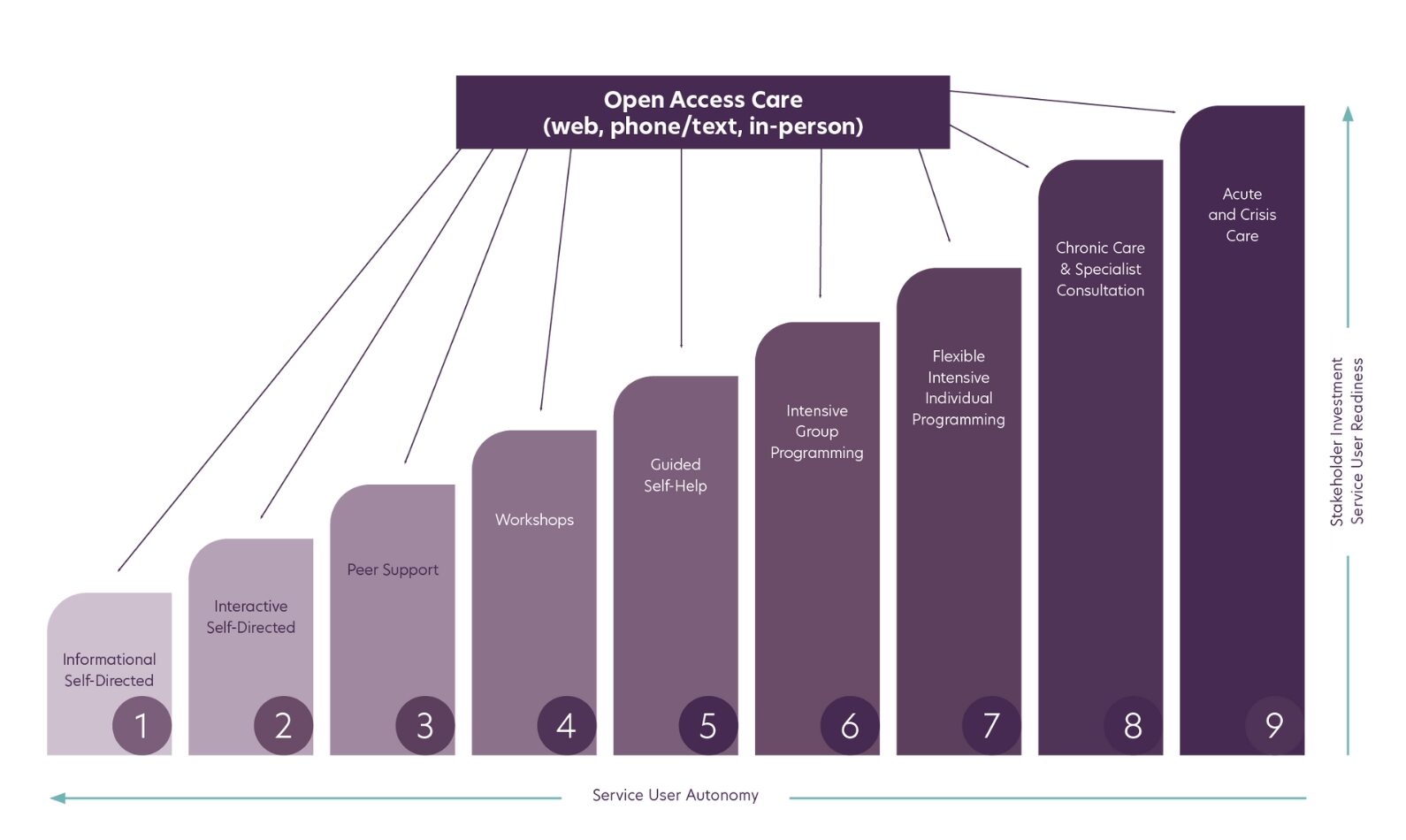
The nine-step framework
The SC2.0 model is organized around 9 steps to capture the full continuum of care, ranging from Step 1: Informational Self-Directed Care to Step 9: Acute Care, Systems Navigation, Case Management & Advocacy.

Community considerations
While each system’s SC2.0 model reflects variability and flexibility in resources and community need, all will include a continuum of service offerings aimed at meeting diverse care seeker needs and will be considered in the “steps” utilized.
STAKEHOLDER INVESTMENT
Stakeholders include people seeking care, service providers, communities, and funders. As intervention intensity increases in the continuum of care, a greater investment of resources such as time, energy and cost is required to achieve optimal results. This is a new way of organizing efforts and all stakeholders need to be on board to make the shift successfully.
CARE SEEKER AUTONOMY
As intervention intensity increases, autonomy for the care seeker decreases. At higher steps, care seekers usually require more assistance and structured programming as in the case of crisis intervention or involuntary hospitalization where autonomy is much lower. At lower steps, they have options for self-guided interventions and learning.
CARE SEEKER READINESS
People seeking services are encouraged to engage with different options to explore those which fit best for their care needs at a given time. As the step levels increase, so too does the requirement for more commitment and care seekers should reflect on their readiness to engage. For example, a peer group may be a good fit for an individual, but they may not be ready to engage in this way.

Putting the model to work for you
Reimagining systems of care takes vision, hard work and commitment. Together, we will co-design a flexible system of care that is responsive to the particular needs of your organization, people who seek services, and the community. We believe that when we come together to reimagine mental health and substance use health care systems, what is produced is truly greater than the sum of its parts.
