
A framework for better, more accessible mental health systems.
Stepped Care 2.0
methodology

Developed in Canada by Dr. Peter Cornish, Stepped Care 2.0© (SC2.0) is an innovative, evidence-informed model for organizing mental health and substance use health services into a co-designed, flexible system of care. Unique in its client-centric and recovery-oriented approach, the model is designed and implemented to fit the needs of diverse organizations and communities. The model can include in-person and virtual modalities, asynchronous and synchronous approaches, as well as self-guided and provider-supported services.
An advanced approach.
Like the UK stepped care model, SC2.0 offers increased access to care at various levels of intensity, with individuals being stepped up or down, as needed. SC2.0 advances the UK model by offering clients informed choice of an extended range of services based on individual needs, preferences and readiness to engage.
Programming is adjusted, in part, given client response and preference, rather than relying on symptom-based, one-size-fits-all rigid treatment protocols. Both client and provider engage in continuous feedback on progress, empowering each to collaborate more on care options and decision-making SC2.0 is designed to create a productive fit between client and care.
OPEN ACCESS
SC2.0 provides flexible, open-access care to help at the point of need and stage of readiness, with minimal assessment.
SYSTEMATIC REACH
SC2.0 creates a system of care that integrates components across the continuum from prevention/promotion to acute care for a whole population approach.
OPEN TO CONTINUOUS IMPROVEMENT
The SC2.0 approach is based on continuous improvement to benefit both providers and people seeking care.
CO-DESIGNED
SC2.0 facilitates a system of care that is co-designed with clients, providers, organizations and the community, resulting in a range of services.
CLIENT-CENTRIC
SC2.0 is recovery-oriented and client-centric.
The nine-step framework.
The SC2.0 model is usually organized around 9 steps to capture the full continuum of care, ranging from Step 1: Informational Self-Directed Care to Step 9: Acute Care, Systems Navigation, Case Management & Advocacy. The implementation of SC2.0 involves organizations selecting services, such as e-mental health interventions, self-guided support, peer support, group programming and in-person therapy, that align with the structure and number of steps appropriate for each community.
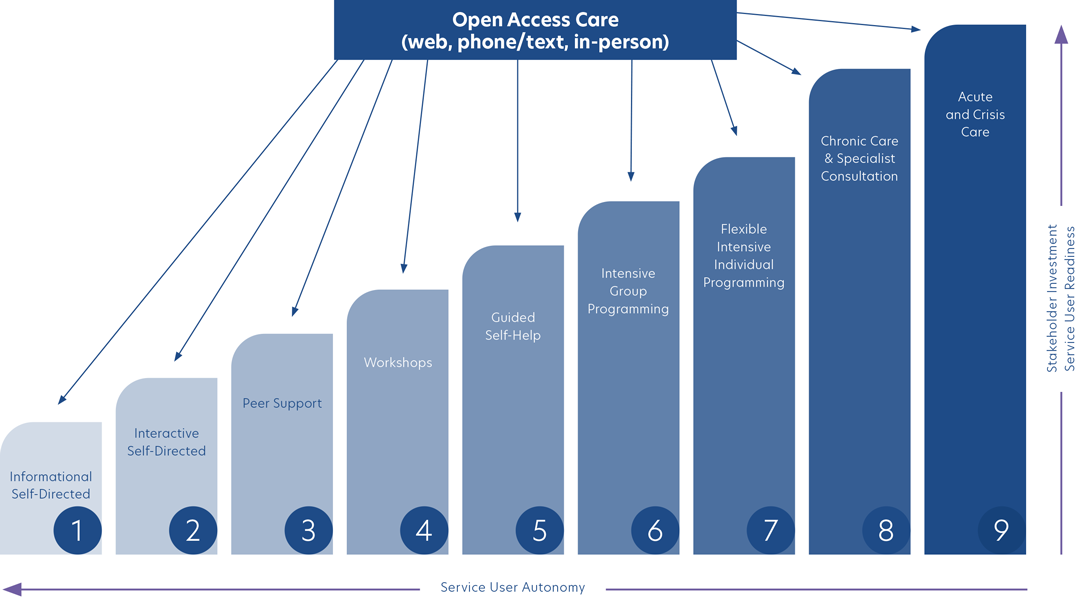
The three factors to be considered for care decisions
While each community’s SC2.0 model will have variability and flexibility when it comes to the services offered, all include a continuum of care aimed at meeting diverse client needs.

STAKEHOLDER INVESTMENT
Stakeholders include help seekers, providers and funders. As intervention intensity increases, a greater investment (i.e., time, effort, and cost) is required to achieve positive results.
SERVICE USER AUTONOMY
As intervention intensity increases, autonomy for the service user decreases. Autonomy is greatest when service users are using lower step informational and self-guided resources. At higher steps, service users require more assistance and structured programming as in the case of crisis intervention or involuntary hospitalization where service user autonomy is much lower.
SERVICE USER READINESS
As step levels increase, a greater commitment is required to achieve expected positive results. For voluntary high intensity programming, clients need to be willing and able to engage in intensive programming.
Putting the Model to Work for You
Together, we will co-design a flexible system of care that is responsive to the particular needs of your organization and community members. Our co-design process is rooted in principles of diversity, equity and inclusion. Every step of the way, care approaches are co-designed to redress inequities within current systems of care.
